HIV testing is a crucial entry point to both HIV prevention and treatment efforts. Early detection through testing allows individuals to know their status, seek timely medical interventions, and adopt preventive measures to reduce the risk of transmission. Testing also plays a pivotal role in connecting people to life-saving antiretroviral therapy (ART) and support services.
For men, who are often part of high-risk populations due to factors such as lower testing rates and higher engagement in certain risky behavior, regular HIV testing, with linkage to prevention or treatment services as appropriate is especially critical.
According to the Kenya Demographic Health Survey 2022, men were less likely to test for HIV/AIDS despite being more likely to have multiple sex partners than women. The document reveals that 67 per cent of men aged 15 to 19 years have never tested while 27 per cent of those aged between 20-24 years do not know about their HIV status. Eleven per cent of men aged 25 to 29 have never been tested, 10 per cent of those between 30 to 34 have never tested, while 15 per cent of men aged 40 to 49, have never been tested. Of the men who have ever had sex, 31 per cent have never tested for HIV.
The Red Carpet Strategy innovation
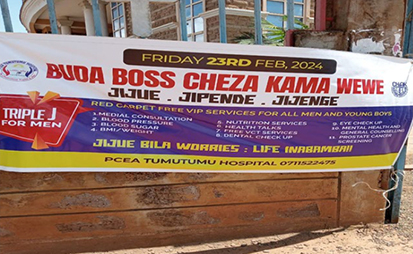
To encourage men to test for HIV, CHAK, through its CHAP Stawisha project implemented an ambitious strategy dubbed the ‘Red Carpet Strategy’. This Differentiated Service Delivery (DSD) approach involves rolling out the red carpet to receive and welcome men seeking health services, simulating a VIP approach to HIV testing and prevention. The strategy seeks to provide a holistic service to improve access, mitigate stigma and ensure value addition by incorporating Non-Communicable Diseases (NCDs) and mental health screening, management and referral into the HIV testing and prevention package.

To implement the strategy, CHAP Stawisha works with high-volume health facilities with over 500-1000 clients current on HIV/AIDS care and treatment. The project also works closely with community leaders who avail spaces such as churches or public grounds for the VIP services, ensuring not only local ownership of the strategy but also cutting costs. Sometimes, the event is held within a health facility.
The process begins with mobilization of the men in the target community for the VIP health services, as they are known. Male champions do the mobilization, reaching out to their fellow men. CHAP Stawisha collaborates with health facilities in the target communities, Community Health Promoters, faith leaders, social and business groups to mobilize the men. The health facilities may print fliers or use other means for mobilization while the Community Health Promoters do door-to-door mobilization. The faith leaders involved also make announcements about the free services during the worship days closest to the Red Carpet Day. Additionally, leaders of social-economic groups, e.g. boda boda and women’s chamas are looped in and asked to sensitize their members on the event. The women play the critical role of relaying information to the men around them. Some women also escort their partners to receive the services.
As the men arrive, they walk on the red carpet to the entry point where they are received and directed to a screening point. At the screening point, those eligible for HIV testing are segregated after being screened for NCDs and mental health. A screening tool is used to determine who is eligible for HIV testing.
Those eligible proceed for HIV testing and blood sugar monitoring. If found to be HIV-negative, the men are initiated on either event-based prep or daily oral prep based on their HIV risk profile, while those identified as HIV-positive are escorted to the health facility to be initiated on ART.
HIV self-test (HIVST) complements existing testing approaches such as the rapid test. Directly Assisted HIV Self Test service delivery approach is utilized during red carpet; trained health service providers and peer educators demonstrate to the client how to perform and interpret the HIVST test. The client then does the self-test and interprets the results. Clients who are found to be HIV-positive are taken through counselling, a confirmation retest using rapid test and treatment started.
The Social Network Strategy (SNS) has been incorporated within the Red-Carpet Strategy to reach more men with HIV services. The SNS strategy is based on the principles that people in the same social network share the same behavior that increases the chances of getting or transmitting HIV, and, in addition, that people in the same social network know and trust each other; summarized as screen me, test me, know my background, identify more people. In the Red-Carpet Strategy, men initiated on PrEP and ART are oriented on SNS and become recruiters who reach out to others who are at substantial ongoing risk of exposure to HIV within their social circles. The recruiters either refer or escort the men for HIV testing during a planned Red Carpet community event or to the facility
The project liaises with the sub-counties to provide condoms during the event where possible.
Red Carpet outcomes
The red carpet strategy has proven to be an effective strategy in reaching men for HIV prevention and treatment services. Through the strategy, a total 4,515 men utilized the VIP services over a 12-month period. A total of 10 New HIV positive clients were identified and initiated on ART, while a further 1,663 men were started on PrEP, an 8-fold increase in PrEP uptake among men.
For diabetes management, hypertension and mental health, referrals are made to the nearest county health facilities. A total of 52 new Hypertension (HTN) clients, 25 new Diabetes Mellitus (DM) clients, and 18 mental health (depression and generalized anxiety disorder) cases have been referred for treatment.
Overall, men express satisfaction and demonstrate high acceptance of the community level VIP services.
Challenges and mitigation measures
A key challenge faced by the strategy is the men not returning to the health facility for retest and PrEP refills. HIV retest is recommended as a follow up to ensure those continuing PrEP are still HIV negative. The program has developed a patient survey questionnaire to elicit patient perceptions of barriers and enablers to male prevention programming, and to complement the client centered red carpet approach, client education and to inform differentiated service delivery that responds to the client unique needs. This survey is administered by the healthcare workers to better understand client's response to the services being offered, understand where, what, and how to improve service provision, understand challenges faced by the clients in accessing services, as well as client's preference on service model to scale up uptake and strengthen retention.
Additionally, there is still low knowledge and awareness about HIV prevention, treatment and care services in communities. For example, most men are unaware of interventions such as event driven Prep (ED Prep) to prevent HIV infection as well as additional bio medical ARV based prevention such as injectable PrEP. Interventions such as the Red Carpet Strategy serve to cascade such knowledge from the facility to the community level.
Next steps
The red carpet strategy has shown demonstrable success, posing a best practice that needs to be scaled up beyond the high volume facilities initially targeted by this initiative, for a men-responsive HIV prevention programming at all levels of the healthcare system. To scale up and replicate this community-based HIV testing and PrEP provision service targeting men, several key steps are essential. First, partnerships with the government, local hospitals, community leaders, and men's groups should be strengthened to ensure culturally sensitive outreach and trust-building. Expanding access points in male-dominated settings such as workplaces, sports clubs, and social venues can increase testing uptake and PrEP access. Providing integrated community HIV services will enhance convenience, appeal and acceptance. Training healthcare providers to deliver gender-sensitive care and addressing stigma around HIV in these communities is vital. Regular monitoring and evaluation of these programs will help adapt strategies, ensuring scalability and sustainability for broader impact.